The Old Cinema Site at Malmesbury, Wiltshire has been surrounded by unanswered questions since its excavation in 2002 (Hart and Holbrook 2011, 166). The uncovering of a medieval cemetery, dating to the 11th to 13th centuries, and the potential remains of a chapel, have raised more questions than answers (Hart and Holbrook 2011, 176). The excavation revealed a maximum of 91 skeletons and two sections of limestone walls. Both have been subject to theories about the people buried in the cemetery and what the building might have once been (Hart and Holbrook 2011). Are these the remains of monks from the neighbouring Malmesbury Abbey, the laity, or a mixture of both? Are the limestone walls the remains of the medieval chapel mentioned by John Leland in 1542 or a later building (Toulmin Smith 1979, 131-132; Hart and Holbrook 2011)?
69 of the 91 skeletons were originally excavated, with the remaining 22 left in situ. Since acquiring these remains, students at the University of York have conducted numerous osteological analyses in search of answers about these people for their dissertation projects. One of these current projects is exploring the topic of degenerative joint disease in the population. The project aims to reveal more information and to uncover the extent to which this particular population was affected by the condition previously provided in the original paper (Hart and Holbrook 2011).
It is difficult to say whether or not more will ever be known about the foundation of the site and who exactly these individuals were and what their role in society was. However, we may still be able to discover what their physical lives were like and what pathologies they may have lived with. This undergraduate dissertation is aimed at understanding the prevalence as well as the correlations between degenerative joint disease and the demography on the site. Not only does the dissertation focus on the presence of degenerative joint disease, it also aims to highlight and address some of the voids in the current methods of evaluation for degenerative joint disease in archaeological populations.
There is surprisingly little known about this site and what structures were present in the medieval period; however this is not the case for the whole town (Luce, 1979; Toulmin Smith 1979; Chandler 1993; Kelly, 2005). The town of Malmesbury in Wiltshire is well known for the 12th century Benedictine Abbey that is currently in ruins (Luce 1979, 29). The abbey brought great attention in its heyday. Unfortunately, this fact did not mean that the history of the town itself and its residents became widely known. There are vast amounts written about the abbey but very little about the surrounding buildings in the town, including other churches (Luce 1979; Kelly 2005). Even one of the greatest historians of his day, William of Malmesbury, who is thought to have spent his whole life in Medieval Malmesbury focuses most of his writing on the abbey, its past and current inhabitants rather than the town (Luce 1979, 22; Burton 1994, 199; Kelly 2005, 32).
The first and one of the only mentions of the site is in 1542 by John Leland during his brief visit to the town; in his manuscript he says:
‘Ther was a litle chirch joining to the south side of the transeptum of thabby chirch... Weavers hath now lomes in this litle chirch, but it stondith and is a very old pece of work’ (Toulmin Smith 1979, 131-132).
This is most probably the structure that the limestone walls found during the excavation represent, as they reside in the location where the excavation took place (Hart and Holbrook 2011, 176). However, it is difficult at this point to say for definite as the church mentioned by Leland may not have even been present in the 11th to 13th centuries.
One of the main benefits of osteoarchaeology, the study of ancient human remains, is that it can shed new light on the lives of people in the past that could not be uncovered in any other way in the archaeological record. On this site in particular it can be very beneficial, as very little is known about these people and what their daily lives may have been like. By looking at the extra-spinal degenerative joint disease in these individuals a tiny flash of light may be shined on these people and we might catch a glimpse of what their lives were like and how similar their ailments could be to ours today.
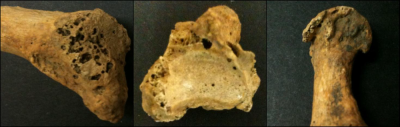
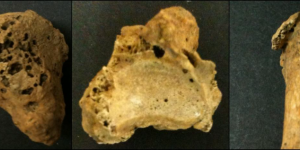
As degenerative joint disease is an age related process, this allowed for all the sub-adult individuals under the age of 18 to be excluded from the study, reducing the number of skeletons from 69 down to 56. Age and sex were both identified where possible for the individuals, using the standard guidelines, as well as all pathologies present on the remains (Brothwell 1981, 72; Lovejoy et al. 1985; Buikstra and Ubelaker 1994, 24-32; White and Folkens 2005). Following this process the presence of degenerative joint disease was assessed. When examining each joint, five diagnostic features were looked for and scored. These features included: porosity (Figure 1), eburnation (Figure 2), central osteophytes (Figure 3), marginal osteophytes, joint surface remodelling, and cysts (Kellgren and Lawrence 1957; Jurmain and Kilgore 1995; Waldron 1995; Waldron and Rogers 1991; Roberts and Manchester 2005).
This dissertation set forth to simply evaluate the presence of degenerative joint disease at the site and to draw comparisons to other contemporary sites, based on the prevalence and the correlations between sex and age in the skeletons affected. However, as the project progressed it became obvious that there was no clear method that could be used in order to consistently label the severity of the condition.
It is after this stage that the process becomes more difficult and subjective. It is easy enough for the symptoms to be identified as present, but it is a completely separate task to assess the severity of the symptom in the individual bones of the joints. Each joint is shaped differently and can be affected by each symptom in a different way, therefore complicating the process of attempting to consistently categorise the symptoms as mild, moderate or severe. For instance, the temporomandibular joint is going to be very differently affected by the disease than the scapula glenoid due to not only the shape of the joint but also the movement that it makes (Rando and Waldron 2012, 45).
This is not the only hindrance in the identification and evaluation of degenerative joint disease. The difficulty addressed so far does not include the actual diagnosis of degenerative joint disease, but rather the identification of symptoms, not all of which have to be present for the diagnosis to be made. However, unlike the identification of symptoms, there is more outside guidance which is moderately more consistent between osteologists that can be relied upon for the actual diagnosis of the condition (Jurmain and Kilgore 1995; Waldron 1997; Rogers and Waldron 1995; Roberts and Manchester 2005; Weiss and Jurmain 2007). The most widespread criteria for diagnosis state that at least two symptoms have to be present for a confident diagnosis to be made. However, there is an exception to this: eburnation is indicative of osteoarthritis—a specific form of degenerative joint disease—independent of all other symptoms due to it being the direct result of bones forming a joint continually rubbing together after the loss of the protective cartilage (Rogers and Waldron 1995). As a result of the formation of eburnation, there can be no other cause aside from a secondary result of trauma which could have been responsible for the osteoarthritis rather than a natural aging or genetic cause (Kellgren et al. 1963; Roberts and Manchester 2005, 138; Weiss and Jurmain 2007).
Although there is a slight variation with regards to the symptoms required by different osteologists to make the diagnosis of degenerative joint disease, there is still a majority that agree. This widely accepted diagnostic criterion requires the previously mentioned combination of symptoms. In the vast majority of published articles on degenerative joint disease in archaeological populations the authors tend to state what criteria they use for determining the presence of degenerative joint disease (DJD) in their study. The struggle is in ensuring that there is a consistency in the severity of each of the symptoms.
There is one definite area of consistency in papers written on the osteological evaluation of DJD, they all say the same thing: there is a “current lack of systematic scoring criteria” (Jurmain and Kilgore 1995, 446). Waldron and Rogers (1991) conducted an experiment to see what variation there was in the coding and diagnosis of DJD in skeletons between beginners and experts. Their results showed that the presence of DJD was quite well recognised. Nonetheless, their experiment also showed that although examiners could identify it, there was a large discrepancy between the severities depending on the examiner: beginners were no better than experts in their agreement of severity (Waldron and Rogers 1991). This subject has been mentioned in numerous papers yet it still has not been rectified (Kelgren and Lawrence 1957; Jurmain 1980, 146; Waldron and Rogers 1991; Jurmain and Kilgore 1995, 446; Rogers et al. 2004). It was mentioned as far back as 1957 in Kellgren and Lawrence’s paper and is still being mentioned in current papers (Weiss and Jurmain 2007).
The judgement of the severity of each diagnostic feature is definitely the most problematic issue in the study. It is very difficult to regulate how an individual defines the terms ‘mild’, ‘moderate’ and ‘severe’. It is one thing to be able to universally identify the presence of the feature and it is a whole other task to consistently categorise the degree of severity.
To help minimise the problem of inconsistency within the evaluation of the skeletons in this project, and to propose a potential starting place for a more strict system to be erected in the future, a strict criteria was implemented. These criteria used specific written descriptions of each symptom in each severity. More than this is truly necessary for reliable assessments to be made that decrease the subjective nature of the study, nevertheless this could be a foundation for a new system.
An additional component of this dissertation steps forth to test the consistency of these criteria similarly to Waldron and Rogers’ project (1991). By testing the criteria with evaluations by a variety of volunteers ranging from beginner to expert - people who had never seen human bones before to someone already an established osteologist - the reliability of the criteria can be tested. The volunteers were provided with not only this written description of symptoms but also a breakdown of pictures showing an unaffected bone in comparison with a bone showing an example of the symptom. The pictures were provided for every level of severity for every symptom with at least one example photo for each.
Although this project headed in a slightly different direction than when it began, it still aims to address all of the objectives established at the start. Nonetheless, it now also aims to suggest a more strict set of guidelines for the evaluation of degenerative joint disease in archaeological populations. The project is reaching its end but has yet to draw any concrete conclusions; by the dissertation deadline in April this project will have shed light on the lifestyles and the evidence of this from the remains, in addition to hopefully bringing attention to, and pushing yet again, for development to be made in the field of archaeological degenerative joint disease identification. One day change will have to come; the field cannot remain stagnant if it wishes to provide efficient and thorough information about past populations.
Bibliography
- Brothwell, D. (1981) Digging Up Bones. Oxford: Oxford University Press
- Buikstra, J.E. and Ubelaker, D.H. (1994) ‘Standards for Data Collection from Human Skeletal Remains’. Arkansas Archaeological Survey. 44
- Burton, J. (1994) Monastic and Religious Orders in Britain 1000-1300. Cambridge: Cambridge University Press
- Chandler, J. (1993) John Leland’s Itinerary: Travels in Tudor England. Gloucestershire: Alan Sutton Publishing
- Hart, J. and Holbrook, N. (2011) ‘A medieval monastic cemetery within the precinct of Malmesbury Abbey: Excavations at the Old Cinema Site, Market Cross’. Wiltshire Archaeological and Natural History Magazine. 104. 166-192
- Jurmain, R.D. (1980) ‘The pattern of involvement of appendicular degenerative joint disease’. American Journal of Physical Anthropology. 53. 143-150
- Jurmain, R.D. and Kilgore, L. (1995) ‘Skeletal evidence of osteoarthritis: a palaeopathological perspective’. Annals of the Rheumatic Diseases. 54. 443-450
- Kellgren, J.H. and Lawrence, J.S. (1957) ‘Radiological assessment of Osteo-Arthrosis’. Annals of the Rheumatic Diseases. 16. 494-502
- Kellgren, J.H., Lawrence, J.S. and Bier, F. (1963) ‘Genetic factors in generalized Osteo-Arthrosis’. Annals of the Rheumatic Diseases. 22. 237-255
- Kelly, S.E. (2005) ‘Charters of Malmesbury Abbey’. Anglo-Saxon Charters. XI
- Lovejoy, C.O., Meindl, R.S., Pryzbeck, T.R. and Mensforth, R.P. (1985) ‘Chronological metamorphosis of the auricular surface of the illium: A new method for the determination of adult skeletal age at death’. American Journal of Physical Anthropology. 68. 15-28
- Luce, R.H. (1979) The History of the Abbey and Town of Malmesbury. Wiltshire: The Friends of Malmesbury Abbey
- Rando, C. and Waldron, T. (2012) ‘TMJ Osteoarthritis: A new approach to diagnosis’. American Journal of Physical Anthropology. 148. 45-53
- Roberts, C.A. and Manchester, K. (2005) The Archaeology of Disease. Stroud: Sutton Publishing. 134-163
- Rogers, J., Shepstone, L. and Dieppe, P. (2004) ‘Is osteoarthritis a systemic disorder of bone?’. Arthritis and Rheumatism. 50 (2). 452-457
- Rogers, J. and Waldron, T. (1995) A Field Guide to Joint Disease in Archaeology. Chichester: Wiley
- Toulmin Smith, L. (1979) Leland’s Itinerary in England and Wales: Volume One. London: Centaur Press Ltd.
- Waldron, H.A. (1997) ‘Association between osteoarthritis of the hand and knee in a population of skeletons from London’. Annals of the Rheumatic Diseases. 56. 85-90
- Waldron. T. (1995) ‘Changes in the distribution of osteoarthritis over historical time’. International Journal of Osteoarchaeology. 5. 385-389
- Waldron, T. and Rogers, J. (1991) ‘Inter Observer Variation in Coding Osteoarthritis in Human Remains’. International Journal of Osteoarchaeology. 1. 49-56
- Weiss, E. and Jurmain, R. (2007) ‘Osteoarthritis Revisited: A contemporary review of aetiology’. International Journal of Osteoarchaeology. 17 (5). 437-450
- White, T.D. and Folkens, P.A. (2005) The Human Bone Manual. Massachusetts: Academic Press